This article provides an in-depth exploration of polycystic ovary syndrome (PCOS), covering its causes, symptoms, and associated risk factors. It emphasizes the significance of understanding the hormonal imbalance underlying PCOS and advocates for a comprehensive approach to management. Lifestyle and dietary strategies are discussed, along with the importance of medical interventions and ongoing support in enhancing quality of life for individuals with PCOS.
PCOS, or polycystic ovary syndrome, is a prevalent hormonal disorder affecting women in their reproductive years. While typically manifesting during adolescence, its symptoms can vary over time.
This condition disrupts hormonal equilibrium, leading to irregular menstrual cycles, heightened androgen levels, and the formation of ovarian cysts. Such irregularities, often stemming from ovulation disturbances, can hinder conception, making PCOS a prominent contributor to infertility.
Though PCOS is chronic and lacks a cure, certain symptoms can be managed through lifestyle adjustments, pharmaceutical interventions, and fertility therapies1.
Understanding the hormonal imbalance in PCOS: causes and effects
The symptoms of PCOS are primarily caused by elevated levels of specific hormones known as androgens. These hormones, produced by the ovaries, are crucial in regulating bodily functions. Among these hormones, estrogen, often called the "female hormone," is predominant in women, while androgens, known as "male hormones," are more abundant in men. Balanced levels of both hormones are essential for overall health in both sexes.
In individuals with PCOS, hormone levels become imbalanced, with heightened androgen levels and possibly reduced estrogen levels. Elevated androgens can disrupt the normal signals from the brain that trigger ovulation, leading to irregular ovulation patterns. They can also halt the development of follicles, the small sacs in the ovaries where eggs mature, causing them to enlarge. Additionally, high androgen levels contribute to other PCOS symptoms like excess hair growth and acne.
Furthermore, PCOS symptoms can also stem from insulin-related issues. Insulin, another important hormone, facilitates the movement of glucose from the bloodstream into cells for energy. When cells become resistant to insulin or fail to respond adequately, blood sugar levels rise. Consequently, the body increases insulin production in an attempt to compensate. Excessive insulin levels can stimulate the production of androgens, exacerbating PCOS symptoms. Moreover, elevated insulin levels may increase appetite, promote weight gain, and contribute to a skin condition called acanthosis nigricans, characterized by darkened patches of skin2.
Risk factors of PCOS
Identifying what exactly causes PCOS is tough because it's a complicated condition influenced by many different things. Factors like pollution, what you eat, your genes, being overweight, and the health of your gut can all be involved. These factors can lead to problems like having too much of the hormone androgen, struggling to respond to insulin properly, difficulties with egg development, and ongoing inflammation in the body. These issues can then increase the chances of developing metabolic syndrome, a cluster of conditions like high blood pressure and high blood sugar that can up the risk of heart disease and diabetes3.
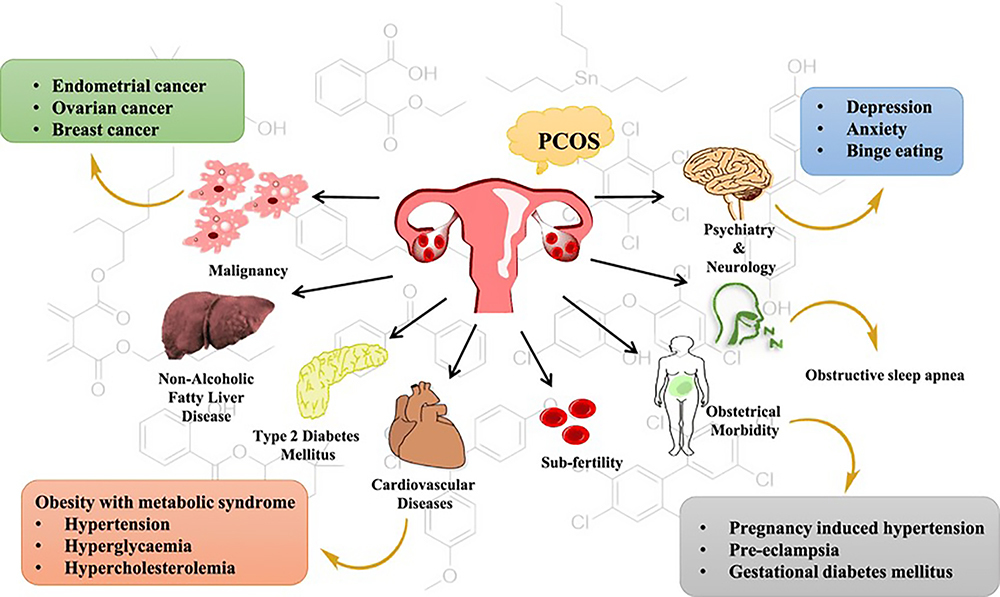
Figure no. 1: Risk factors of PCOS.
Symptoms of PCOS
PCOS, or polycystic ovary syndrome, presents a range of symptoms that can impact various aspects of a person's health and well-being. One common manifestation is irregular or infrequent menstrual cycles, where periods may occur at prolonged intervals or cease altogether. Additionally, some individuals with PCOS experience episodes of heavy or prolonged bleeding during menstruation, which can be disruptive and distressing.
Hair-related symptoms are also prevalent among those with PCOS. While scalp hair may become noticeably thinner, excess hair growth, known as hirsutism, can occur on areas such as the upper lip, chin, chest, back, abdomen, arms, and legs. This excessive hair growth can be a source of embarrassment and self-consciousness for many individuals.
Weight management can be particularly challenging for those with PCOS, with many individuals struggling to lose weight, especially around the abdominal area. This abdominal obesity is not only a cosmetic concern but also increases the risk of developing other health complications associated with PCOS.
Skin-related symptoms are common as well, including oily skin and acne, which can affect one's appearance and self-esteem. Moreover, a condition called acanthosis nigricans may occur, characterized by darkening of the skin, typically seen on the neck and in the armpits.
PCOS can also have significant implications for fertility and pregnancy. Infertility is a common issue, as irregular ovulation can make it difficult to conceive. Those with PCOS also face an increased risk of miscarriage and may experience complications during pregnancy, such as gestational diabetes.
Beyond the physical symptoms, PCOS can take a toll on mental health. Depression and anxiety are frequently reported among individuals with PCOS, possibly stemming from the emotional challenges associated with infertility, body image concerns, and hormonal imbalances.
Furthermore, inflammation is believed to play a role in PCOS and can manifest as joint pain, muscle aches, and fatigue. These symptoms can further impact one's quality of life and overall well-being, making the management of PCOS a multifaceted endeavor that requires comprehensive care and support1,4.
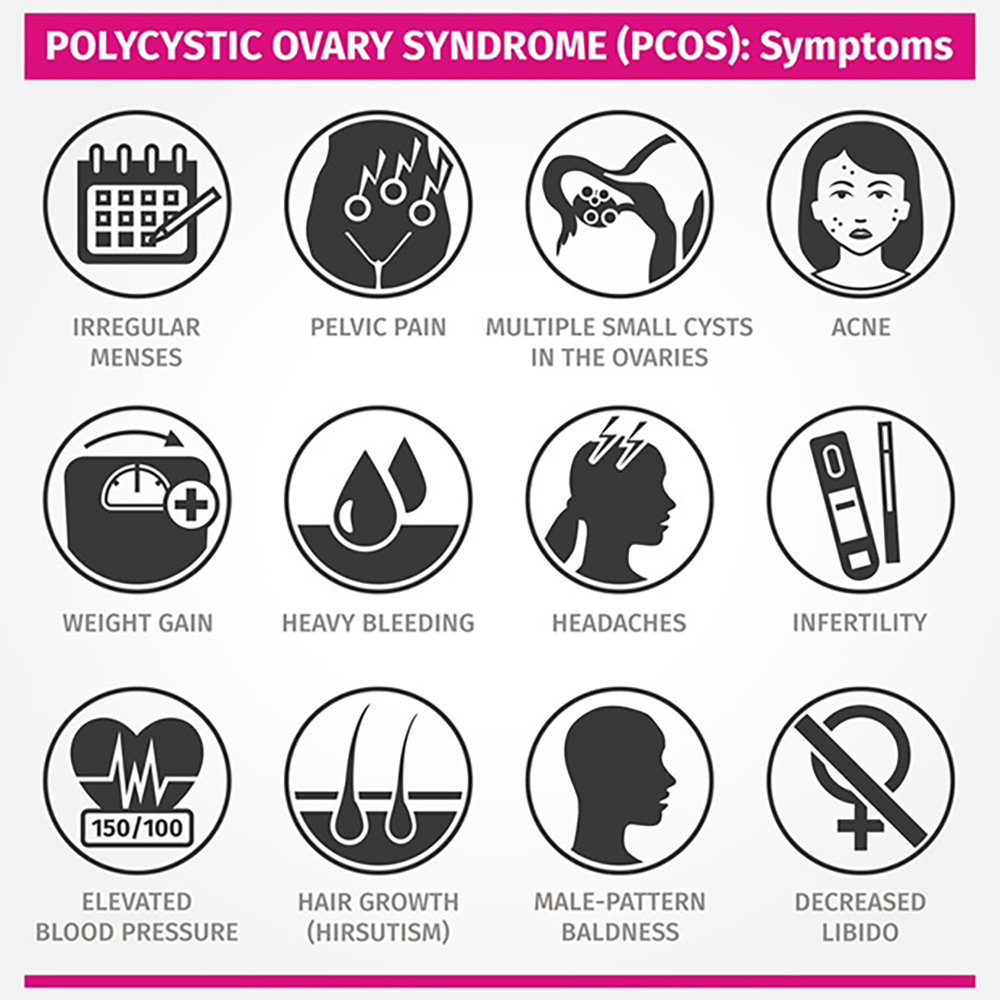
Figure no. 2: Symptoms of PCOS.
Lifestyle and dietary management of PCOS
Lifestyle modifications
Treating PCOS often involves a multifaceted approach, including lifestyle adjustments to manage symptoms and enhance overall health. The primary aim is to attain or sustain a healthy weight, as excess weight can exacerbate PCOS symptoms and elevate the risk of complications5.
Weight management
Striving for a weight reduction of 5–10% is advised for individuals with excess weight, as this may result in improvements in PCOS symptoms. Lifestyle interventions, such as dietary modifications and increased physical activity, have demonstrated efficacy in achieving weight loss and enhancing reproductive outcomes in PCOS5.
Exercise
Regular physical activity is a crucial component of PCOS management. Exercise not only aids in weight loss but also enhances insulin sensitivity and cardiovascular health. Aim for at least 150 minutes of moderate-intensity exercise per week, or as recommended by a healthcare professional.
Dietary strategies
While there is no universal diet for PCOS, certain dietary strategies can help ameliorate symptoms and promote overall well-being.
Carbohydrate modification
Adopting low glycemic index (GI) or low glycemic load (GL) diets may be advantageous for individuals with PCOS. These dietary patterns can assist in regulating blood sugar levels, improving insulin sensitivity, and reducing appetite, thereby facilitating better weight management and reproductive outcomes6.
Protein intake
Increasing protein consumption may help suppress androgen levels and enhance insulin sensitivity in individuals with PCOS. High-protein diets have been shown to reduce weight, waist circumference, and fat mass, while also improving metabolic markers and reproductive hormones6.
Fat composition
Prioritize the consumption of healthy fats, such as monounsaturated fatty acids (MUFA) and polyunsaturated fatty acids (PUFA), found in foods like nuts, seeds, and fatty fish. These fats can enhance insulin sensitivity and lipid profiles, potentially lowering the risk of cardiovascular disease in individuals with PCOS6.
Dietary patterns
Various dietary patterns, including the Dietary Approaches to Stop Hypertension (DASH) diet and vegetarian or vegan diets, have been linked to improvements in PCOS symptoms. These dietary approaches are rich in fiber, plant proteins, and antioxidants, which can support metabolic health and hormonal balance 6.
Key insights for navigating PCOS management
In summary, the management of polycystic ovary syndrome (PCOS) requires a comprehensive and individualized approach that goes beyond simple lifestyle adjustments and dietary changes. It involves a holistic strategy that integrates medical interventions, lifestyle modifications, and ongoing support.
Firstly, medical interventions such as pharmaceutical treatments and fertility therapies play a crucial role in addressing specific symptoms and underlying hormonal imbalances associated with PCOS. These may include medications to regulate menstrual cycles, reduce androgen levels, and improve insulin sensitivity. Fertility treatments such as ovulation induction medications may also be prescribed for those trying to conceive.
Secondly, lifestyle modifications are essential components of PCOS management. These include adopting a balanced diet, engaging in regular physical activity, managing stress levels, and prioritizing adequate sleep. These lifestyle changes not only help in weight management but also contribute to improving overall health and well-being.
Furthermore, ongoing support from healthcare professionals, such as endocrinologists, gynecologists, and nutritionists, is crucial for individuals with PCOS. Regular monitoring of symptoms, hormonal levels, and treatment efficacy allows for timely adjustments to the treatment plan as needed. Additionally, education and counseling can help individuals better understand their condition and develop coping strategies to navigate its challenges.
In conclusion, managing PCOS effectively requires a comprehensive and collaborative approach that addresses the multifaceted nature of the condition. By combining medical interventions, lifestyle modifications, and ongoing support, individuals with PCOS can achieve better symptom control, improved fertility outcomes, and an enhanced quality of life.
References
1 World Health Organization. (n.d.). Polycystic ovary syndrome.
2 National Institute of Child Health and Human Development. (n.d.). What causes polycystic ovary syndrome (PCOS)?
3 ResearchGate. (n.d.). The risk factors of polycystic ovary syndrome (PCOS).
4 University Health News. (n.d.). 12 PCOS symptoms: This complex disease involves more than ovarian cysts.
5 Singh, S., Pal, N., Shubham, S., Sarma, D. K., Verma, V., Marotta, F., & Kumar, M. (2023). Polycystic Ovary Syndrome: Etiology, Current Management, and Future Therapeutics. Journal of clinical medicine, 12(4), 1454.
6 Bhattacharya, S., Singh, A., & Pal, R. (2022). Dietary Strategies for the Management of Polycystic Ovary Syndrome: A Comprehensive Review. BMC Endocrine Disorders, 22(1), 56.















