A better understanding of how aging promotes CVD is therefore urgently needed to develop new strategies to reduce the disease burden. Atherosclerosis and heart failure contribute significantly to age-associated CVD-related morbimortality. CVD and aging are both accelerated in patients suffering from Hutchinson-Gilford progeria syndrome (HGPS), a rare genetic disorder caused by the prelamin A mutant progerin. Progerin causes extensive atherosclerosis and cardiac electrophysiological alterations that invariably lead to premature aging and death. This review summarizes the main structural and functional alterations to the cardiovascular system during physiological, neurological, motor, and somatic issues due to aging is the time-related, progressive functional decline that affects all organ systems.
It is believed to be caused by the accumulation of DNA damage, hormonal changes, and internally programmed cellular changes. Effects of aging include stiffening of the arteries and calcification of valves (cardiovascular system), osteoporosis and increased risk of fracture (musculoskeletal system), decreased chest wall compliance and increased ventilation-perfusion mismatch (respiratory system), susceptibility to recurrent infections and malignancies (immune system), and decline in cognitive function and changes in sleep patterns (nervous system).
Blood flows through our veins and arteries with each heartbeat, supplying our bodies with nutrition and oxygen. However, as we age, the system may become more prone to inflammation, blood vessels may stiffen, and blockages may accumulate. These factors raise the risk of heart attacks, heart failure, and other cardiac problems. Lifestyle decisions, our surroundings, and our genetic makeup can all affect how well our hearts function. According to research, women's risk of cardiovascular disease increases significantly after menopause, although males have a higher risk than women when they are younger. Tufts University School of Medicine researchers are attempting to ascertain the reasons for these variations and the most effective ways to support us in maintaining our cardiovascular health as we age.
Discussion
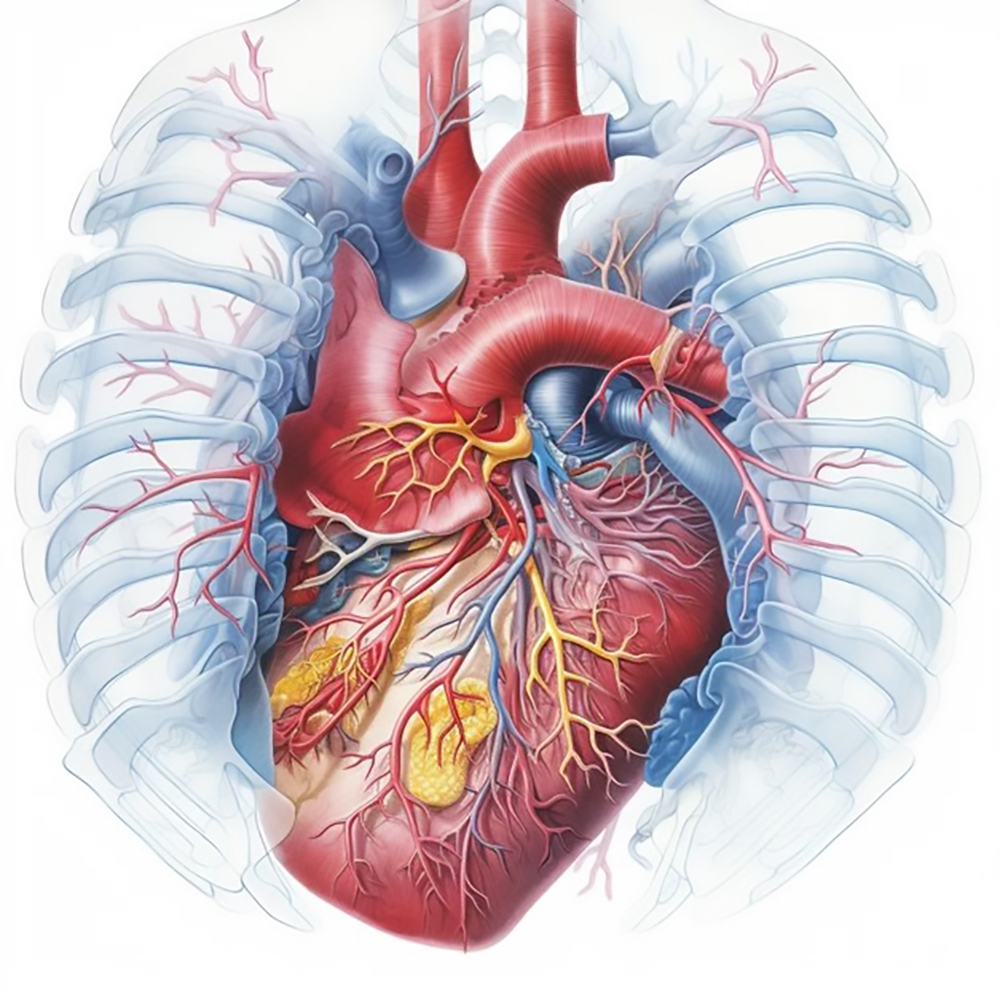
Your cardiovascular system ages along with your skin and hair. Even with healthy cardiovascular systems, changes in the heart and arteries can occur as early as age 20. This can include changes in the heart's structure and/or rhythm, thickening of the arteries and heart valves, and more. The left side of the heart pumps oxygen-rich blood around the body, while the right side pumps blood . to the lungs to take in oxygen and remove carbon dioxide. Your arteries leave your heart, branching and narrowing until they reach your tissues, where they eventually become microscopic capillaries. Oxygen and nutrients are delivered through capillaries.
Capillaries carry oxygen and nutrients to tissues and return carbon dioxide from there. The carbon dioxide is then transported to larger and larger blood vessels, which return the blood to the heart. However, the risk of heart problems increases slowly as you age because of normal aging-related changes in your cardiovascular system, such as a slightly slower heart rate due to fibrous tissue and fatty deposits that form in the body's natural heart rhythm system, which regulates the heartbeat. The natural pacemaker (SA node) also loses some of its cells. The heart fills more slowly due to the thickening of the heart wall, so the heart chamber can hold less blood. Shrinking and thickening of the heart valves, which control the direction of blood flow and the heart wall.
This can reduce the heart's tolerance to exercise and other stresses. Thickening of the walls of small capillaries, which can slow the exchange of nutrients and waste, Aorta flexibility, stiffness, and thickening are reduced, which can lead to hypertension. rise and strengthen the heart. Decreased production of white blood cells, or neutrophils, which are important for certain immunity. This can reduce your ability to fight infections. Red blood cell production slows during stress or illness, resulting in a slower response to blood loss and anemia.
As we age, several changes occur in our cardiovascular system. Some of the key changes include
1. Arterial stiffening
The walls of our arteries become less flexible and more rigid with age, leading to increased blood pressure and reduced blood flow to organs and tissues.
Arterial stiffening is a common age-related change that occurs in the cardiovascular system. As we age, the walls of our arteries become less elastic and more rigid, leading to increased blood pressure and reduced blood flow to organs and tissues. This process is known as arteriosclerosis, or arterial stiffness. Arterial stiffening is primarily caused by the accumulation of collagen and other proteins in the walls of the arteries, which leads to decreased flexibility and compliance. This can result in several negative effects on cardiovascular health, including:
Increased blood pressure: Stiff arteries are less able to expand and contract in response to changes in blood flow, leading to higher blood pressure. Elevated blood pressure is a major risk factor for cardiovascular diseases such as heart attack, stroke, and heart failure.
Reduced blood flow: Stiff arteries can impair the ability of the arteries to dilate and constrict in response to changing demands for blood flow. This can lead to reduced blood flow to organs and tissues, potentially causing damage and dysfunction. Increased workload on the heart: Arterial stiffening can increase the workload on the heart as it pumps blood against higher resistance in the stiffened arteries. This can contribute to left ventricular hypertrophy (thickening of the heart muscle) and increase the risk of heart failure. Impaired baroreflex function: Baroreceptors are specialized nerve endings in the walls of the arteries that help regulate blood pressure by sensing changes in pressure and signaling the body to adjust accordingly.
Arterial stiffening can impair the function of these baroreceptors, leading to dysregulation of blood pressure control. Management of arterial stiffening typically involves lifestyle modifications such as regular exercise, maintaining a healthy weight, following a balanced diet low in salt and saturated fats, managing stress, and avoiding smoking. In some cases, medications may be prescribed to help control blood pressure and reduce the risk of cardiovascular events. Regular monitoring of blood pressure and cardiovascular health by a healthcare provider is important for the early detection and management of arterial stiffening and its associated risks. By taking proactive steps to maintain cardiovascular health, individuals can reduce the impact of arterial stiffening and age-related changes on their overall well-being.
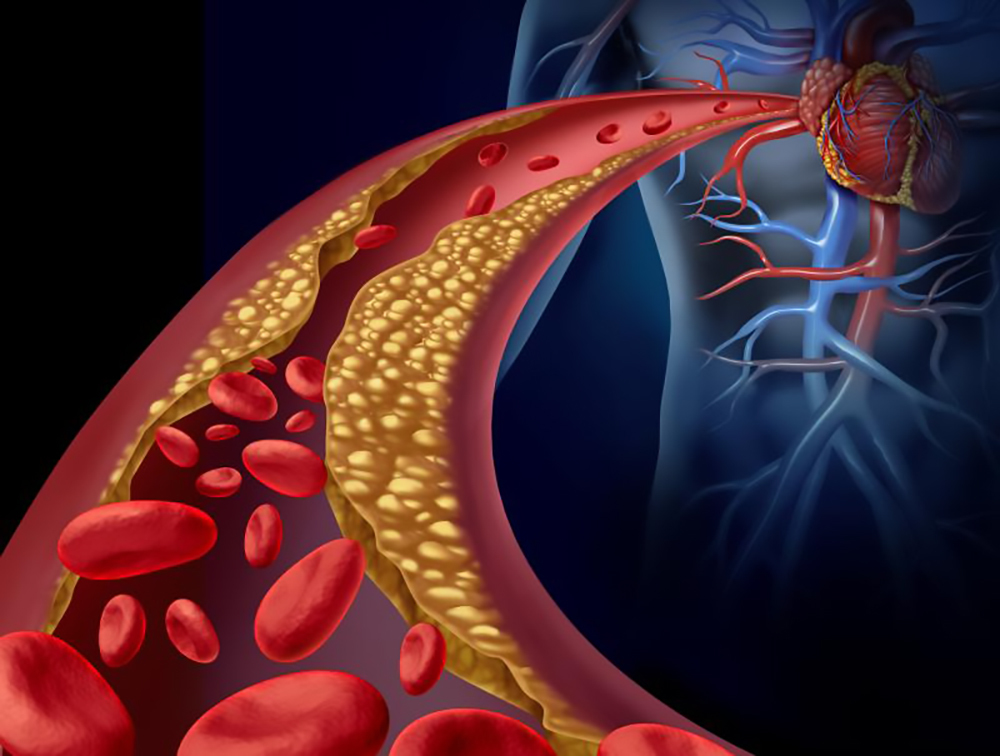
2. Artheroeclerosis
The build-up of plaque in the arteries, a condition known as atherosclerosis, becomes more common with age. This can lead to the narrowing of the arteries and increase the risk of heart attack and stroke. Arteriosclerosis is a broad term that refers to the thickening and hardening of the walls of arteries. It is a natural part of the aging process and can have significant implications for cardiovascular health. There are three main types of arteriosclerosis: Atherosclerosis: This is the most common type of arteriosclerosis and involves the buildup of plaque (made up of cholesterol, fats, calcium, and other substances) on the inner walls of arteries. Over time, this plaque can narrow and harden the arteries, restricting blood flow and increasing the risk of heart attack, stroke, and other cardiovascular problems.
Monckeberg's arteriosclerosis: This type of arteriosclerosis primarily affects medium-sized arteries and is characterized by calcification (calcium deposits) in the middle layer of the arterial wall. While it may not always lead to significant narrowing of the arteries, it can still contribute to reduced elasticity and increased stiffness. Arteriolosclerosis: This type of arteriosclerosis affects small arteries and arterioles (smaller branches of arteries). It is often associated with conditions like hypertension (high blood pressure) and diabetes. Arteriolosclerosis can lead to thickening and narrowing of these small vessels, impacting blood flow to organs and tissues.
As we age, the walls of our arteries naturally become stiffer and less elastic due to changes in the composition of the arterial walls, including the accumulation of collagen and other proteins. This arterial stiffening can contribute to increased blood pressure, reduced blood flow to vital organs, and an overall decline in cardiovascular function.
In addition to age-related changes, lifestyle factors such as poor diet, lack of exercise, smoking, and stress can accelerate the progression of arteriosclerosis. Managing these risk factors through healthy lifestyle choices and regular medical check-ups can help mitigate the impact of arteriosclerosis on cardiovascular health. Treatment for arteriosclerosis typically focuses on managing risk factors, such as controlling blood pressure and cholesterol levels, maintaining a healthy weight, quitting smoking, and exercising regularly. In some cases, medications or procedures may be recommended to address specific issues related to arterial stiffness or blockages. Regular monitoring and early intervention are key to managing arteriosclerosis in aging individuals and reducing the risk of serious cardiovascular complications. By taking proactive steps to protect heart health, individuals can improve their quality of life and reduce the burden of age-related arterial changes.
3. Cardiac heart muscle
The heart muscle may thicken and become stiffer with age, which can affect its ability to pump blood efficiently.
As we age, changes occur in the structure and function of cardiac muscle, which can impact overall cardiovascular health. Some of the key changes in cardiac muscle associated with aging include:
Cardiac hypertrophy: with age, the heart may undergo hypertrophy, which is the thickening of the walls of the heart chambers, particularly the left ventricle. This can be a compensatory response to increased workload or changes in blood pressure. However, excessive hypertrophy can lead to impaired heart function and an increased risk of heart failure.
Fibrosis: aging is associated with an increase in fibrosis, which is the accumulation of collagen and other proteins in the heart muscle. Fibrosis can lead to stiffening of the heart muscle, impairing its ability to relax and contract effectively. This can contribute to diastolic dysfunction, where the heart has difficulty filling with blood properly.
Reduced cardiac output: as we age, there is a gradual decline in cardiac output, which is the amount of blood pumped by the heart per minute. This decrease in cardiac output is primarily due to changes in heart rate and stroke volume (the amount of blood ejected with each heartbeat). It can affect exercise capacity and overall cardiovascular function.
Impaired electrical conduction: aging can also affect the electrical conduction system of the heart, leading to alterations in heart rhythm (arrhythmias), such as atrial fibrillation. These changes can increase the risk of cardiovascular events like stroke or heart attack.
Decreased response to stress: the ability of the aging heart to respond to stress, such as physical activity or emotional stress, may be reduced. This can impact the heart's ability to adapt to changing demands and maintain optimal function.
Mitochondrial dysfunction: mitochondria are the energy-producing organelles within cells, including cardiac muscle cells. With aging, there may be a decline in mitochondrial function, leading to decreased energy production and potential oxidative stress within cardiac muscle cells. Managing these age-related changes in cardiac muscle is crucial for maintaining cardiovascular health and reducing the risk of heart disease. Lifestyle factors such as regular exercise, a healthy diet, weight management, stress reduction, and avoiding smoking can help support heart health as we age. Additionally, regular medical check-ups, monitoring blood pressure and cholesterol levels, and following recommended treatments for cardiovascular conditions are essential for managing age-related changes in cardiac muscle and promoting overall heart health.
4. Decline in cardiac rate variability
The variability in heart rate, which is an indicator of the heart's ability to respond to stress, tends to decrease with age. Heart rate variability (HRV) refers to the variation in time intervals between consecutive heartbeats, which reflects the autonomic nervous system's regulation of the heart. HRV is an important indicator of cardiovascular health and overall well-being. As we age, there is a gradual decline in heart rate variability, which can have implications for cardiovascular function and overall health.
Autonomic nervous system changes: the autonomic nervous system plays a crucial role in regulating heart rate variability. With aging, there is a decrease in the flexibility and responsiveness of the autonomic nervous system, leading to a reduction in HRV. This decline can affect the heart's ability to adapt to stressors and maintain optimal function.
Increased sympathetic dominance: as we age, there is often an increase in sympathetic nervous system activity and a decrease in parasympathetic activity. This shift towards sympathetic dominance can result in reduced heart rate variability, as sympathetic activation tends to produce a more regular and less variable heart rate pattern.
Cardiovascular risk factors: age-related changes in heart rate variability are associated with an increased risk of cardiovascular disease, including hypertension, arrhythmias, and heart failure. Lower HRV has been linked to a higher risk of adverse cardiovascular events and mortality.
Physical fitness: regular physical activity and exercise can help maintain or improve heart rate variability, even as we age. Exercise has been shown to enhance autonomic function, increase parasympathetic tone, and improve HRV. Incorporating aerobic exercise, strength training, and flexibility exercises into your routine can support cardiovascular health and HRV.
Stress management: chronic stress can negatively impact heart rate variability by increasing sympathetic activity and reducing parasympathetic activity. Practicing stress-reducing techniques such as mindfulness, meditation, deep breathing exercises, and yoga can help improve HRV and overall cardiovascular health.
Sleep quality: adequate sleep is essential for maintaining optimal heart rate variability. Poor sleep quality or sleep disorders can disrupt the balance of the autonomic nervous system and lead to decreased HRV. Establishing good sleep habits and addressing any sleep-related issues can support healthy heart rate variability. Monitoring heart rate variability through wearable devices or specialized tests can provide valuable insights into cardiovascular health and overall well-being, especially as we age. By adopting a healthy lifestyle, managing stress, staying physically active, and prioritizing good sleep habits, it is possible to support heart rate variability and promote cardiovascular health throughout the aging process.
5. Changes in conductive system
The electrical system that controls the heartbeat may become less efficient with age, leading to irregular heart rhythms. The aging process can lead to changes in the conductive system of the heart, which is responsible for coordinating the electrical signals that regulate the heart's rhythm and contractions. These changes can impact the heart's ability to function effectively and may increase the risk of arrhythmias and other cardiac conditions. Here are some key changes in the conductive system of the heart that occur with aging:
Fibrosis: with age, there is an increase in fibrosis within the heart's conduction system. Fibrosis is the formation of excess connective tissue, which can disrupt the normal propagation of electrical impulses through the heart. This can lead to delays or blockages in conduction, resulting in arrhythmias or conduction abnormalities.
Calcification: the accumulation of calcium deposits within the heart's conduction system can also occur with aging. Calcification can stiffen the cardiac tissues and interfere with the transmission of electrical signals, leading to conduction disturbances and impaired heart function.
Degeneration of pacemaker cells: the specialized cells within the heart's conduction system that generate electrical impulses (such as the sinoatrial node) may undergo degenerative changes with age. This can affect the heart's ability to initiate and regulate its rhythm, potentially resulting in bradycardia (slow heart rate) or other rhythm abnormalities.
Impaired conduction velocity: age-related changes in the structure and function of cardiac muscle fibers can slow down conduction velocity within the heart. This can lead to delays in signal transmission between different regions of the heart, increasing the risk of arrhythmias and synchronization issues.
Increased risk of arrhythmias: The alterations in the conductive system associated with aging can predispose individuals to various types of arrhythmias, such as atrial fibrillation, atrioventricular block, or ventricular tachycardia. These arrhythmias can disrupt the heart's normal rhythm and potentially compromise cardiac function.
Electrophysiological changes: aging can also affect the electrophysiological properties of cardiac cells, including changes in ion channel function and action potential duration. These alterations can contribute to arrhythmogenesis and impact the heart's responsiveness to external stimuli.
Management and Treatment: it is important for older individuals to undergo regular cardiac evaluations, including electrocardiograms (ECGs) and Holter monitoring, to assess their heart's conduction system function. Depending on the findings, interventions such as medications, pacemakers, or other electrophysiological procedures may be recommended to manage arrhythmias and maintain optimal heart function.
By understanding the changes that occur in the conductive system of the heart with aging, healthcare providers can implement appropriate strategies to monitor and address potential cardiac issues in older adults. Maintaining a healthy lifestyle, managing cardiovascular risk factors, and seeking timely medical care can help mitigate the impact of age-related changes on the heart's conduction system.
6. Increase risk of heart desease
Aging is a major risk factor for cardiovascular diseases such as coronary artery disease, heart failure, and arrhythmias.
Aging is a major risk factor for the development of heart disease, as the cardiovascular system undergoes various structural and functional changes over time. The aging process can contribute to the accumulation of risk factors and the progression of underlying cardiovascular conditions, increasing the likelihood of heart disease in older individuals. Here are some key factors that contribute to the increased risk of heart disease with aging:
Atherosclerosis: aging is associated with the progressive buildup of plaque within the arteries, a condition known as atherosclerosis. This narrowing and hardening of the arteries can restrict blood flow to the heart muscle, leading to coronary artery disease and an increased risk of heart attacks and angina.
Hypertension: the prevalence of high blood pressure tends to rise with age, as blood vessels become less flexible and more resistant to blood flow. Uncontrolled hypertension can strain the heart, increase the risk of heart failure, and contribute to the development of other cardiovascular complications.
Dyslipidemia: changes in lipid metabolism and cholesterol levels can occur with aging, leading to dyslipidemia characterized by elevated levels of LDL cholesterol and triglycerides. These lipid abnormalities can promote atherosclerosis and raise the risk of cardiovascular events.
Diabetes: aging is a significant risk factor for type 2 diabetes, a condition characterized by insulin resistance and high blood sugar levels. Diabetes is a major risk factor for heart disease, as it accelerates atherosclerosis, increases inflammation, and impairs cardiac function.
Obesity: the prevalence of obesity tends to increase with age, contributing to a higher risk of heart disease. Excess body weight can lead to metabolic abnormalities, such as insulin resistance and inflammation, that promote the development of cardiovascular conditions.
Sedentary lifestyle: older adults may become less physically active over time, which can contribute to weight gain, muscle loss, and a decline in cardiovascular fitness. A sedentary lifestyle is associated with an increased risk of heart disease and other chronic conditions.
Stress and mental health: aging can be accompanied by changes in mental health, including increased stress, anxiety, and depression. Psychological factors can impact cardiovascular health, contributing to hypertension, arrhythmias, and other heart-related issues.
Family history and genetics: genetic factors play a significant role in determining an individual's risk of heart disease. Aging individuals with a family history of cardiovascular conditions are at higher risk of developing similar issues themselves.
Medication use: older adults often take multiple medications for various health conditions, which can interact with each other and affect cardiovascular function. Certain medications may have side effects that increase the risk of heart disease or worsen existing cardiac conditions.
Lifestyle factors: smoking, poor diet, excessive alcohol consumption, and other unhealthy lifestyle choices can further elevate the risk of heart disease in aging individuals. Given the complex interplay of these factors, it is essential for older adults to prioritize heart-healthy behaviors and undergo regular cardiovascular screenings to detect and manage potential risk factors early on. Lifestyle modifications, such as maintaining a healthy diet, engaging in regular physical activity, managing stress, quitting smoking, and controlling chronic conditions like hypertension and diabetes, can help mitigate the risk of heart disease in aging individuals. Additionally, working closely with healthcare providers to monitor cardiovascular health and address any emerging issues promptly is crucial for maintaining optimal heart function and overall well-being as we age.
It is important to maintain a healthy lifestyle, including regular exercise, a balanced diet, and avoiding smoking and excessive alcohol consumption, to help preserve cardiovascular health as we age. Regular check-ups with a healthcare provider are also important to monitor and manage any cardiovascular risk factors.
Cardiovascular disease in physiological aging
Changes The following subsections summarize the main functional and structural changes that occur in the heart during normal aging. Heart failure. Heart failure (HF) is a complex clinical syndrome strongly associated with aging and caused by some structural or functional defect of ventricular filling or ejection that results in inadequate perfusion of peripheral tissues. Clinical manifestations of HF include dyspnea and fatigue, limited exercise capacity, and fluid retention, which can cause pulmonary and/or peripheral edema. In a large proportion of elderly patients, the ejection fraction remains unchanged, indicating preservation of total systolic function. Therefore, age-related heart failure in otherwise healthy individuals is more likely to be due to left ventricular diastolic filling dysfunction. Impaired systolic function and left ventricular dysfunction occur when the LV loses its ability to relax normally due to myocardial stiffness due to fibrosis.
Left ventricular hypertrophy (LVH), which is characterized by an increase in LV wall thickness, is more common in men and women (28–30) as they age and is a strong independent predictor of death and morbidity, particularly in the elderly (28, 31). Age-related left ventricular hypertrophy (LVH) is caused by a gradual pathologic remodeling of the heart that includes collagen deposition, cardiomyocyte enlargement, and death. Independent factors that have been recognized as potentially causing the development of LVH include blood pressure, obesity, valve dysfunction, and myocardial infarction. Heart failure. The extracellular matrix's (ECM) increasing collagen content with aging is linked to cardiac fibrosis and the emergence of LVH.
Still, little is known about the exact mechanisms behind age-related cardiac remodeling. As people age, it has been suggested that the primary cause of cardiac fibrosis in hypertension is not increased collagen synthesis but rather the downregulation of matrix-degrading pathways and increased collagen cross-linking. In order to replace lost heart tissue, fibrosis is also triggered. Fibrosis increases the age-related incidence of LV and heart valve dysfunction and arrhythmias by impairing the myocardium's ability to conduct electrical impulses, relax and stretch properly, and diffuse oxygen. This makes fibrosis a major risk factor for mechanical and electrical dysfunction in HF.
Concluding remarks and perspectives
Aging is the predominant risk factor for CVD. Because societies are progressively aging, and CVD is the main cause of morbidity worldwide, we urgently need to improve our knowledge of the mechanisms underlying tissue and organismal aging. This information is critical to the development of new strategies to reduce disease burden in the elderly and thus promote healthy aging. Intense efforts in basic, clinical, and epidemiological research have identified general mechanisms implicated in aging. These were recently classified into primary hallmarks of aging (genomic instability, telomere attrition, epigenetic alterations, and loss of proteostasis) that trigger antagonistic hallmarks (deregulated nutrient sensing, mitochondrial dysfunction, and cellular senescence), leading to integrative hallmarks (stem cell exhaustion and altered intercellular communication).
A challenge in aging research is to identify which of the aging hallmarks contributes most to explaining the high interindividual variability in human biological aging, as well as to understand their relative contribution to age-associated cardiovascular damage. This knowledge should help researchers develop new therapies and improve prevention by identifying individuals at higher risk of suffering age-related diseases before symptoms appear, thus promoting healthy aging and reducing the health care and socioeconomic impacts of aging.
(This article was written with contribution of Alejandra Marin Hernandez)
References
1 Aging in the Cardiovascular System: Lessons from Hutchinson-Gilford Progeria Syndrome.
2 How does the cardiovascular system change with age?
3 What Happens to our Cardiovascular System as We Age?